
Back and limb pain is one of the most common diseases.This is the second largest medical cause after respiratory disease.About half of working-age people in their lifetime will endure the attacks of back pain and long-term disability.
What is osteochondral disease
Osteochondrosis is a disease of disc degeneration.
The intervertebral disc consists of the center annulus (the concentric layer of the strong connective tissue fibers) and the outer core.The share of the intervertebral discs accounts for about a quarter of the length of the spine, and they act as shock absorbers - a fibrous river with vertical positions, turns, tilts and extensions of the spine, nucleus and intervertebral discs, which occupies the stop of the axial load, which occupies the starting position.There is a significant load on the discs of the lumbar and cervical spine because these departments have the greatest mobility.This explains the fact that cervical and lumbar spine degeneration is the most serious.
One of the reasons for disk degeneration is their inadequate nutrition, which in turn is the result of a person's physical exercise.
The water content and elastic properties of the disk also decrease significantly with age.The fiber rings of the disk lose their elasticity, and cracks appear in it, where, at each new load, the jacket core begins to introduce more and more into the jacket core, moving to the edge of the disk, the entire fiber ring is broken, and everything in the core exceeds its limits - beyond the source of the jacket core.Lateral displacement of the intervertebral disc is more common and occurs in the direction of the vertebrae through which the spinal cord passes.In this regard, the most common manifestation of hernia is the development of the corresponding root and characteristic pain syndrome.Under the influence of pulses from receptors of affected fragments, when the spinal muscle reflexes, their asymmetric stress can lead to the transverse curvature of spinal fissures when the spinal fissure is reflexive.
Risk factors for osteochondrosis
Currently, risk factors for the occurrence of osteocartilage and opaque pain include:
- genetic weakness or congenital defects in the spine;
- spinal injury that causes structural changes;
- Heavy and unbalanced physical exercise;
- Stay in forced poses of twisting and turning for a long time;
- Hypoemia, inactivity, monotonous work.
Osteochondrosis and its deterioration may occur in various infectious diseases, cooling, overwork, power disorders, including vitamin deficiency, obesity, environmental factors and habits, endocrine diseases, etc.
What to do if your back is sick
Pain is a warning sign that can be protected from harm from the effects on the body.First, pain occurs when moving, changing posture and passing at rest, and morning stiffness occurs as the disease progresses, which can last for 30-60 minutes.The duration of the disease may be weeks or months.
What to do if you have a back injury?Be sure to consult a doctor within the first 3-5 days (to avoid chronological dynasties).In addition to the doctor's advice, simple tips should be used:
- Overload should be avoided.To avoid problems, try constantly monitoring the correct position of your body.Excess weight can increase the load on the spine.Not all sports are the same.It is best to avoid playing sports, jumping and opting for hiking, snowboarding and swimming – they only benefit the spine.
- Correctly organize sleep, food and rest.For maximum results, choose a rather tough mattress, and an orthopedic pillow will be the best choice.
- Organize your workplace correctly.The seat with a low and tilted rear seat should be convex in the lumbar position (or a roller is recommended).
- Location processing.A very high roller is installed under the lower back spine, the "tensive" muscles are relaxed, the back pressure of the damaged lumbar disc is reduced, and the pain is reduced.After working days, it is recommended to spend 30-60 minutes at this location at home before bed.
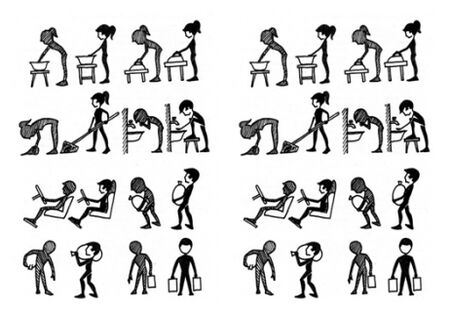
- Treatment of gymnastics (exercise therapy).Gymnastics creates a strong muscle corset around the spine, and 15-25 minutes per day for 15-25 minutes (you can use 2-3 methods).A set of exercises should be prescribed by the treatment physician based on the intensity of the pain, and at the end of this article we will provide the most common therapeutic exercise complex based on the period of the disease (acute stage, remission, etc.).
Suggestions for exercise patterns in acute periods
In acute periodsIn the presence of acute pain, strict bed rest should be observed.LFK is primarily used for sanitary purposes and is essentially a universal enhancement.Exercises that cause pain should be subject to exercises that are amplitude, muscle tone level or radically excluded.It is important to not participate in pain and do it very slowly, repeating 8-10 times per exercise is very important.
When moving the lower limbs, prevent the increase in the lumbar forelimbs (curving the spine forward), thereby enhancing pain syndrome.In the second phase of the acute period, as the intensity of the pain decreases, you should carefully include isometric exercises to train your abdominal muscles and large gluteus muscles.
Pain syndrome decreasesThe possibility of using special and developmental exercises is increased.During this period, in addition to exercises that increase the strength of the abdominal and hip muscles, exercise is important, with lumbar flexion.
When choosing special exercises and development exercises, it is important to make sure they do not increase the lumbar muscles.Pain is a signal that exercises structural changes (to relieve) or eliminates pain.At the end of the second phase, you should gradually include exercises to increase the strength of your back muscles, which can be performed 2-3 times in a circular system.They are the most important.The number of repetitions for special exercises is 15-50 times.The speed of movement can be gradually increased.
During the remission periodExercises were added to increase spinal mobility.However, exercises designed to solve this problem should be carefully performed in a lightweight starting position.Automation should achieve automation by maintaining specific postures in standing positions and walking when the lumbar spine is bent.Repeat replies for the second phase of special exercises to 50-100 times (may be damaged during the day).It is recommended to use exercise therapy in the pool during this period, but gymnastics in the pool cannot replace it, but instead supplement the main "dry" category.
In another method of exercise therapy, it is recommended to use methods that do not affect the negative ways of damaged discs: swimming, tetanus, snowboard, running paths, bicycle measurement tables, exercises with rubber bandages.Use volleyball, tennis (size and size), road bicycle, cross-country running, fast dancing, rhythmic gymnastics and other methods, as sudden movements and turns will cause the aggravation of bone cartilage.It is best to do dumbbell exercises while lying (back, abdomen) to eliminate vertical load on the spine.
Exercise and throwing on the rowing machine is undesirable due to the intense tension of the body's stretched muscles, jumping into the depth of the elevation, so using pure suspension is undesirable.In any case, during exercise therapy, the ongoing damage and overload of the spine should be kept in mind, and the impact along the spinal axis prepares appropriate background for the collapse of the damaged intervertebral disc and the aggravation of pain syndrome.























